Examining the value-based care approach: How improved data models and analysis can remedy inequities - MedCity News
Over the past decade healthcare providers have increasingly adopted value-based care (VBC) approaches, a move fueled greatly by the 2010 passage of the Affordable Care Act (ACA), as well as the recognition of the exorbitant costs of medical care, and the racial and socioeconomic inequities in healthcare access.
VBC is tied to various alternative payment models (APM) that shift healthcare provider reimbursement from a fee-for-service (FFS) to payment models driven by quality of care—some more dramatically so than others. Data supporting both improved patient outcomes and cost-effectiveness of VBC had begun to mount when the Covid-19 pandemic disrupted healthcare systems and revealed that many APMs, as currently structured, don’t benefit healthcare providers operating under trying conditions and serving high-risk communities—that is, those working in environments and with populations where new approaches to healthcare are most needed.
While the revelation of structural economic issues has led to some question the inherent viability of VBC, it’s worth first exploring potential tweaks to and supplementary tools for APMs that could resolve these inequities. When we peek under the hood, we see that some economic flaws of VBC may be caused by all too familiar blind spots about the impacts of socioeconomic status and health that influence the metrics used to evaluate the performance and govern the reimbursement of healthcare providers using these APMs. Correcting those underlying presumptions and improving data analysis on the part of healthcare providers could go a long way to mitigating the economic risks for providers who embrace VBC.
What went wrong with VBC during the pandemic?
In the early stages of the pandemic, it seemed that Covid-19 would manifest as a catalyst for healthcare providers to transition to APMs. Value-based providers fared well early in the pandemic; they had more flexibility to quickly integrate telehealth tools and approaches to avoid disruption in patient care and, unlike FFS providers, had existing mechanisms to bill payers for such services. But over time, the pandemic revealed two key vulnerabilities of VBC and APMs in terms of ability of care providers to earn equitable reimbursement.
The first issue with VBC in light of the pandemic is that APMs determine reimbursement based on measures in established domains—effectiveness, efficiency, timeliness, safety, patient focus, and equitability. The practical realities of delayed or deferred care, as the pandemic lingered, led to worsening outcomes, increased infectious complications, and higher mortality—and costs—for patients across a range of diseases.
These dynamics hurt providers’ performance on APMs’ defined metrics, labeling care as inefficient, less effective, and less timely. In some instances, under certain APMs, defined quality measurements must be reached before care providers can receive payment. These metrics and requirements, to which FFS providers are not subject, seem especially strict in an environment in which unmet quality standards can credibly be attributed to external conditions as opposed to the VBC approach itself or the performance of a care provider. Further, while the pandemic primarily impacted patient care in 2020-2021, quality measures relying on 2020 data will impact hospital quality reporting and payment programs for years to come, meaning the financial repercussions of this shortcoming of APMs could have a long tail for those who adopted VBC frameworks.

The second issue with reimbursement under APMs is that the racial and socioeconomic health disparities of the patients get unfairly reflected in—or rather, falsely attributed to—the “performance” of those providers. This bug most harshly punishes the bottom line of providers who treat patients at greatest risk. For example, due to socioeconomic factors, the likelihood of persons of color contracting Covid-19 is as much as three times higher than White individuals and suffer from higher mortality rates from Covid-19. Therefore, the risks of unrecouped costs for service due to the circumstances prompted by the extreme events like the pandemic are most acute for care providers who disproportionately serve the highest-need populations.
As a result of these dynamics, some care providers who initially embraced VBC-are beginning to revert to a more FFS-centric approach.
Reexamining presumptions inherent in VBC payment structures
The stresses of the pandemic highlighted that VBC and their associated APM affect providers differently, most severely hurting those that serve high-risk communities. But, there’s an opportunity to lean on improved modeling, analytics, and data to improve the inequities of the system.
For example, “risk scores” currently used to adjust spending measures fail to recognize important differences in patient needs and can thereby mislabel physicians and hospitals as “inefficient” if they care for patients who have acute illnesses or complex problems, or have simply not been able to seek care due to an external force, like a pandemic. Operationally speaking, different payers may rely on different quality measurements, and those measurements may unintentionally codify socioeconomic biases within payment models that skew in favor of providers treating lower-risk communities. Re-examining the underlying presumptions built into the APMs could identify structural biases and opportunities to correct the models.
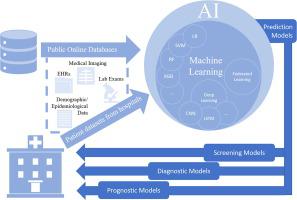
On the provider end, comprehensive, advanced analytic platforms, and digital tools can help track patient progress, measure success, and drive down cost. Once providers understand how a VBC program and the associated APMs work, along with their capacity to operate within it, they can better quantify risk and identify opportunities to efficiently improve outcomes. However, data entry and analysis can be time-consuming and confusing, and inputting incomplete or inaccurate data can result in patient progress going uncaptured and providers being shortchanged. The opportunities to better utilize these tools to ensure adequate reimbursement is present for all providers, but especially for primary care providers.
At a minimum, providers should be trained to integrate tools like EHRs, care coordination platforms, and patient health management platforms into their care and patient management. They also need to get educated on how important correctly capturing and analyzing data is to ensure they’re compensated for the full value of their services.
Further, many digital tools are being developed that can support a transition to VBC. From tools like Eyton Health that leverage data integration, machine learning and analytic automation to scale, connect and analyze health data to improve performance and financial outcomes, to those like the Enlace Technology Platform and SiftMD that help optimize billing and collections for value-based payers, care providers looking to optimize the economics of a shift to VBC have a growing selection of tools to aid the transition.
Meanwhile, software developers should continue to simplify tools, improving the user experience, so programs will be used properly and completely. Improving software, data capture and analysis can help protect against fraud as well, making it more difficult to game the system through practices like falsifying the underlying patient risk levels to misrepresent the impact and financial value of service.
A value-based future
The underlying premise and commitments of VBC remain laudable and the approach retains potential to cost-effectively improve patients’ outcomes, especially in high-risk communities. But for care providers to continue to buy in, the economics must work for all parties involved and remain viable amid circumstances that quickly and profoundly impact the healthcare environment—like a pandemic.
Unfortunately, the models underlying many of the associated APMs may reflect some of the same blind spots to which society at large is prone—judging the disadvantaged and those who treat them with incomplete context, misinterpreting circumstantial obstacles preventing compliance as underperformance and personal or institutional inadequacy. APMs’ sensitivity to the impacts of Covid-19 is itself something of a microcosm of this same shortcoming, as the impact of the pandemic was, too, a shift in patient behavior driven by circumstance, not individual or institutional failure.
By building greater understanding of context and flexibility into APMs and enabling providers to make data-driven choices, we can begin to address inequities burdening VBC and help ensure APMs remain viable and enticing for healthcare providers.
Photo: Hong Li, Getty Images
Promoted
It’s clear that life science companies need to transform their approach to be much more collaborative in the way they work with healthcare professionals.
Microsoft and MedCity News
Promoted
For researchers who aren’t affiliated with an academic library, finding scientific papers can be time-consuming and expensive—and organizing and sharing them with co-workers can be even harder. A new tool by DeepDyve looks to help researchers address this gap.
DeepDyve Digital Library Team